Topic how long do period headaches last: Discover the duration and relief strategies for period headaches, a common yet often misunderstood issue. This comprehensive guide delves into their causes, duration, and effective treatments, offering insights and solutions for those affected.
Table of Content
- How long do period headaches typically last?
- Causes of Period Headaches
- Duration of Period Headaches
- Identification and Diagnosis
- Treatment Options
- Impact of Hormonal Birth Control
- YOUTUBE: Menstrual Migraine and Period Headaches: Causes and Solutions
- Preventive Strategies and Lifestyle Tips
- Risk Factors and Complications
How long do period headaches typically last?
Period headaches, also known as menstrual migraines, usually occur around the time of a woman\'s menstrual cycle and can last for several days. The duration of these headaches can vary depending on the individual, but on average, they typically start two days before the period begins and continue until the third day of the period.
- Step 1: The headaches, called menstrual migraines, typically start two days before the period begins.
- Step 2: They continue throughout the menstrual cycle.
- Step 3: The headaches usually last until the third day of the period.
- Step 4: The duration may vary for each person, but symptoms can last for a few hours or even several days.
It\'s important to note that approximately 70% of people who experience migraines are women, suggesting a connection between hormonal changes during the menstrual cycle and the occurrence of period headaches.
READ MORE:
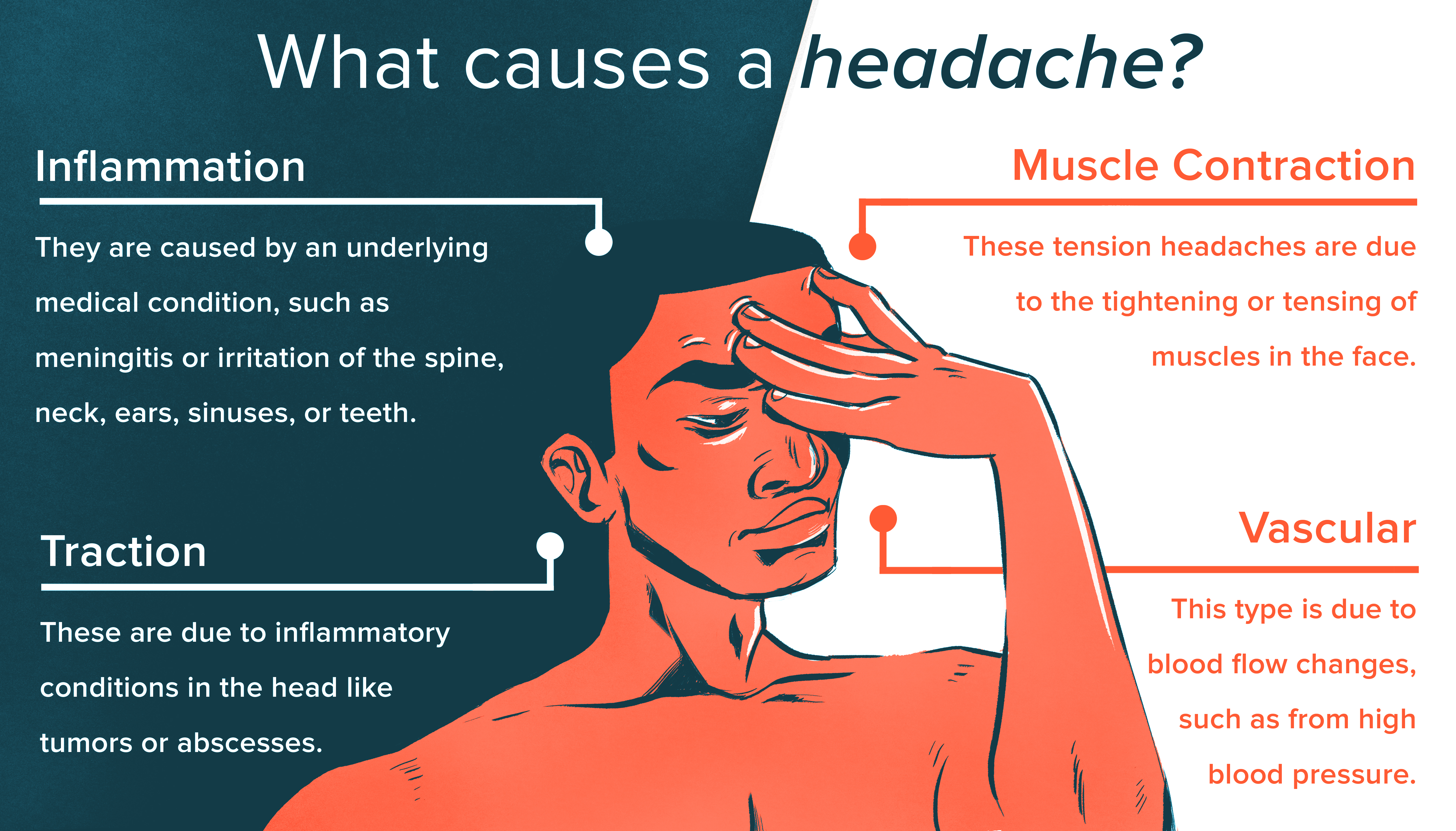
Causes of Period Headaches
Period headaches, commonly referred to as menstrual migraines, are primarily caused by hormonal fluctuations in the body. These headaches often begin due to a rapid decline in estrogen levels just before the onset of menstruation. Additionally, prostaglandins, which are chemicals produced in the lining of the uterus, also play a significant role in triggering these headaches.
- Estrogen Decline: A sharp drop in estrogen levels is a primary trigger for menstrual migraines.
- Prostaglandins Role: These chemicals, produced in the uterus, contribute to the development of headaches during menstruation.
- Family History: Individuals with a family history of migraine headaches are more likely to experience menstrual migraines.
Understanding these triggers is crucial for both individuals and healthcare providers to manage and possibly anticipate the occurrence of menstrual migraines effectively. Keeping a detailed migraine journal can be particularly helpful in identifying the specific causes and patterns of these headaches.
:max_bytes(150000):strip_icc()/what-is-a-menstrual-migraine-1719930_v2-3cca14811df0401fb429e9d738c53a5a-4f27a94438104586ad86fe57135d2d5d.png)
Duration of Period Headaches
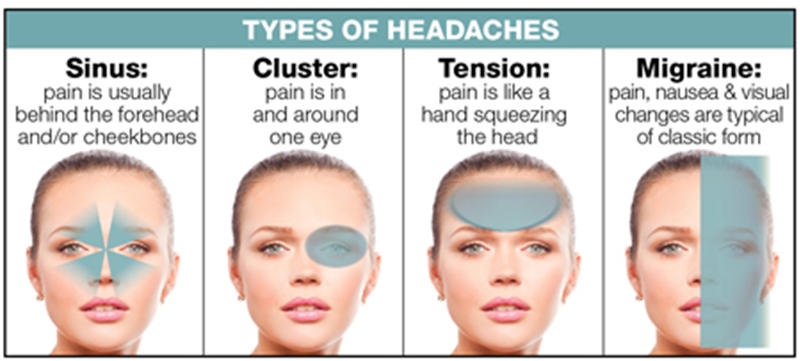
Period headaches, often associated with menstrual migraines, have a specific duration pattern linked to the menstrual cycle. They typically commence a couple of days before the onset of menstruation and can persist until the third day of the menstrual period. These headaches are characterized by intense throbbing or pulsing in one area of the head and may include symptoms like nausea, vomiting, and sensitivity to light and sound.
- Start Time: Usually 2 days before menstruation begins.
- Duration: Can last through the menstrual period, often until the third day.
- Symptom Intensity: These headaches may present more severe symptoms than non-menstrual migraines and might be less responsive to usual migraine treatments.
It"s important to note that the duration and intensity can vary among individuals. Keeping a headache journal can be a useful tool for tracking the specific patterns and severity of menstrual migraines, aiding in effective management and treatment planning.
Identification and Diagnosis
Identifying and diagnosing period headaches, particularly menstrual migraines, involves a comprehensive approach. Key to this process is understanding the unique symptoms and triggers associated with these headaches.
- Symptom Recognition: Menstrual migraines typically manifest as intense throbbing or pulsing in one area of the head, accompanied by nausea, vomiting, and sensitivity to light and sound. These symptoms usually begin two days before the period and last until the third day of menstruation.
- Migraine Journal: Keeping a detailed journal of headache symptoms, their duration, and potential triggers is vital. This journal helps in identifying patterns and specific characteristics of menstrual migraines.
- Medical Evaluation: Healthcare providers may recommend blood tests, imaging tests like CT scans or MRIs, and sometimes an electroencephalogram (EEG) to rule out other causes and confirm the diagnosis.
- Hormonal Factors: As menstrual migraines are linked to hormonal changes, particularly the rapid fall in estrogen levels, healthcare providers might also consider hormonal factors during diagnosis.
Effective diagnosis is a collaborative process between individuals and healthcare providers, using both self-recorded data and professional medical assessment to accurately identify and treat menstrual migraines.

Treatment Options
Treatment for menstrual migraines and period headaches varies based on severity and individual response. The goal is to alleviate symptoms and prevent future occurrences.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs like Ibuprofen, Naproxen, and Ketoprofen are often used. Starting treatment two to three days before the period and continuing during menstruation can help manage symptoms.
- Triptans: These are selective serotonin receptor agonists used for acute migraines. Medications like Sumatriptan and Zolmitriptan are common choices. They are taken after the onset of a migraine to halt its progression.
- Hormonal Treatments: Hormonal contraceptives can stabilize estrogen levels, reducing the frequency of menstrual migraines. Continuous use, skipping the placebo week, can be beneficial for some women.
- Lifestyle Adjustments: Regular sleep patterns, stress management, and maintaining a balanced diet can also help manage menstrual migraines.
- Other Medications: Depending on individual cases, doctors might prescribe beta-blockers, anticonvulsants, or calcium channel blockers. In some instances, supplements like estrogen or other specific treatments may be recommended.
It is essential to work with a healthcare provider to determine the best treatment plan based on personal health history and migraine patterns.
Impact of Hormonal Birth Control
Hormonal birth control methods, such as the pill, patch, ring, or intrauterine system, can significantly impact headaches and migraines associated with menstrual cycles. These methods work by regulating hormone levels in the body, particularly estrogen, which can fluctuate during the menstrual cycle and trigger headaches.
During the estrogen-free intervals of certain hormonal birth control regimens, some individuals may experience an increase in headaches or migraines. This is due to the sudden drop in estrogen levels, similar to the natural drop that occurs before menstruation. However, for some, hormonal birth control can help reduce the frequency and severity of period-related headaches by stabilizing hormone levels throughout the cycle.
- Continuous or Extended-Cycle Regimens: Skipping the placebo days or using extended-cycle birth control pills can minimize or eliminate the hormone-free intervals, potentially reducing the occurrence of headaches.
- Non-Oral Hormonal Contraceptives: Methods such as the hormonal IUD, patch, or ring can also help maintain stable hormone levels and may be beneficial for those who experience migraines with aura, although they should be used with caution and under medical advice.
- Monitoring and Adjustment: It"s crucial for individuals starting a new hormonal contraceptive to monitor their headache patterns and work with their healthcare provider to adjust the method if headaches increase or do not improve.
Ultimately, the impact of hormonal birth control on headaches can vary widely among individuals. Some may find relief, while others may experience an increase in headache frequency or intensity. Close monitoring and communication with a healthcare provider are essential to finding the most suitable method for managing headaches related to the menstrual cycle.
:max_bytes(150000):strip_icc()/Verywell_Perimenopause_And_Migraines_4009311_V1-09d5bbe3e80e4980b23f3efbed2afb84.jpg)
Menstrual Migraine and Period Headaches: Causes and Solutions
\"This 5-minute video will provide you with all the important information you need in just a short duration! Discover practical tips and techniques to make the most out of your time and increase productivity.\"
Preventive Strategies and Lifestyle Tips
Maintaining a healthy lifestyle can significantly reduce the frequency and severity of period-related headaches. The following strategies and tips can help manage and prevent these headaches:
- Regular Exercise: Engaging in regular physical activity, such as walking, swimming, or yoga, can help reduce the severity and frequency of headaches. Exercise promotes overall well-being and stress reduction.
- Stress Management: Techniques such as meditation, deep-breathing exercises, and mindfulness can help manage stress levels, which may trigger headaches during menstruation.
- Sleep Hygiene: Maintaining a regular sleep pattern and ensuring adequate rest can help prevent headaches. Aim for 7-9 hours of quality sleep per night.
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and may reduce headache occurrences. Avoiding processed foods, excessive caffeine, and alcohol can also be beneficial.
- Hydration: Staying well-hydrated is essential for overall health and can help prevent headaches. Aim to drink at least 8 glasses of water per day.
- Magnesium Supplements: Some studies suggest that magnesium deficiency may be linked to headaches. Consider adding magnesium supplements to your diet after consulting with a healthcare provider.
- Avoid Trigger Foods: Certain foods may trigger headaches in some individuals. Keeping a food diary can help identify and avoid these triggers.
Implementing these lifestyle changes can not only help in managing period-related headaches but also contribute to overall health and well-being. It"s important to start with small, manageable changes and gradually incorporate them into your daily routine for the best long-term results.
Hormonal Migraine and Period Headaches: Causes and Treatment Options
\"Looking for a natural and effective treatment for your skin? Look no further! In this video, you\'ll learn about a groundbreaking treatment that will help you achieve clear and glowing skin in no time.\"
READ MORE:
Risk Factors and Complications
Understanding the risk factors and potential complications associated with period-related headaches is essential for effective management and prevention. Here are some key points to consider:
- Family History of Migraines: A family history of migraines increases the likelihood of experiencing menstrual migraines, suggesting a genetic predisposition.
- Hormonal Fluctuations: Significant hormonal changes, especially the drop in estrogen levels before menstruation, are a major trigger for menstrual migraines.
- Migraine with Aura: Individuals who experience migraine with aura may have an increased risk of certain complications, such as an increased risk of stroke, particularly if they smoke or use combined hormonal contraceptives.
- Use of Combined Hormonal Contraceptives: While hormonal contraceptives can help manage menstrual migraines for some, they may increase the risk of stroke in individuals with migraine with aura. It"s crucial to discuss the risks and benefits with a healthcare provider.
- Overuse of Medication: Frequent use of headache medication can lead to medication overuse headaches, worsening the headache pattern over time.
It"s important to consult with a healthcare provider for a proper diagnosis and to discuss potential risk factors and complications related to period-related headaches. Managing risk factors, monitoring symptoms, and following a tailored treatment plan can help minimize the impact of menstrual migraines on daily life.
Explore our comprehensive guide on period headaches to understand their duration, causes, and effective treatment strategies, empowering you to manage and overcome these discomforts for a healthier, more comfortable menstrual cycle.






:max_bytes(150000):strip_icc()/VWH_Illustration_Natural-Remedies-for-Managing-Headaches_Paige-McLaughlin_Final-461a780622884c479edf3dc01234692c.jpg)


:max_bytes(150000):strip_icc()/VWH_Illustration_Getting-Rid-of-a-Migraine_Illustrator_Ellen-Lindner_Final-a245985cbf4645a7874d573991fb6cbb.jpg)