Topic why do i get bad headaches on my period: Experiencing bad headaches during your period? You"re not alone. This article delves into the causes of menstrual migraines and offers practical advice for relief, empowering you to manage these discomforts more effectively.
Table of Content
- Why do headaches occur during menstruation?
- Overview of Menstrual Headaches
- Hormonal Fluctuations and Their Impact
- Identifying Menstrual Migraines
- Lifestyle Factors and Triggers
- Effective Home Remedies
- Medical Treatments and Pain Relief
- YOUTUBE: How to alleviate headaches during menstruation
- When to Consult a Healthcare Professional
- Preventive Strategies and Lifestyle Modifications
Why do headaches occur during menstruation?
Headaches during menstruation, commonly known as menstrual migraines, are a significant concern for many women. These migraines are often triggered by hormonal changes that occur during the menstrual cycle.
Here are the key points explaining why headaches occur during menstruation:
- Hormonal fluctuations: The drop in estrogen levels that happens before menstruation can trigger migraines in some women.
- Changes in serotonin levels: Serotonin levels tend to fluctuate during the menstrual cycle. Low serotonin levels are associated with migraines.
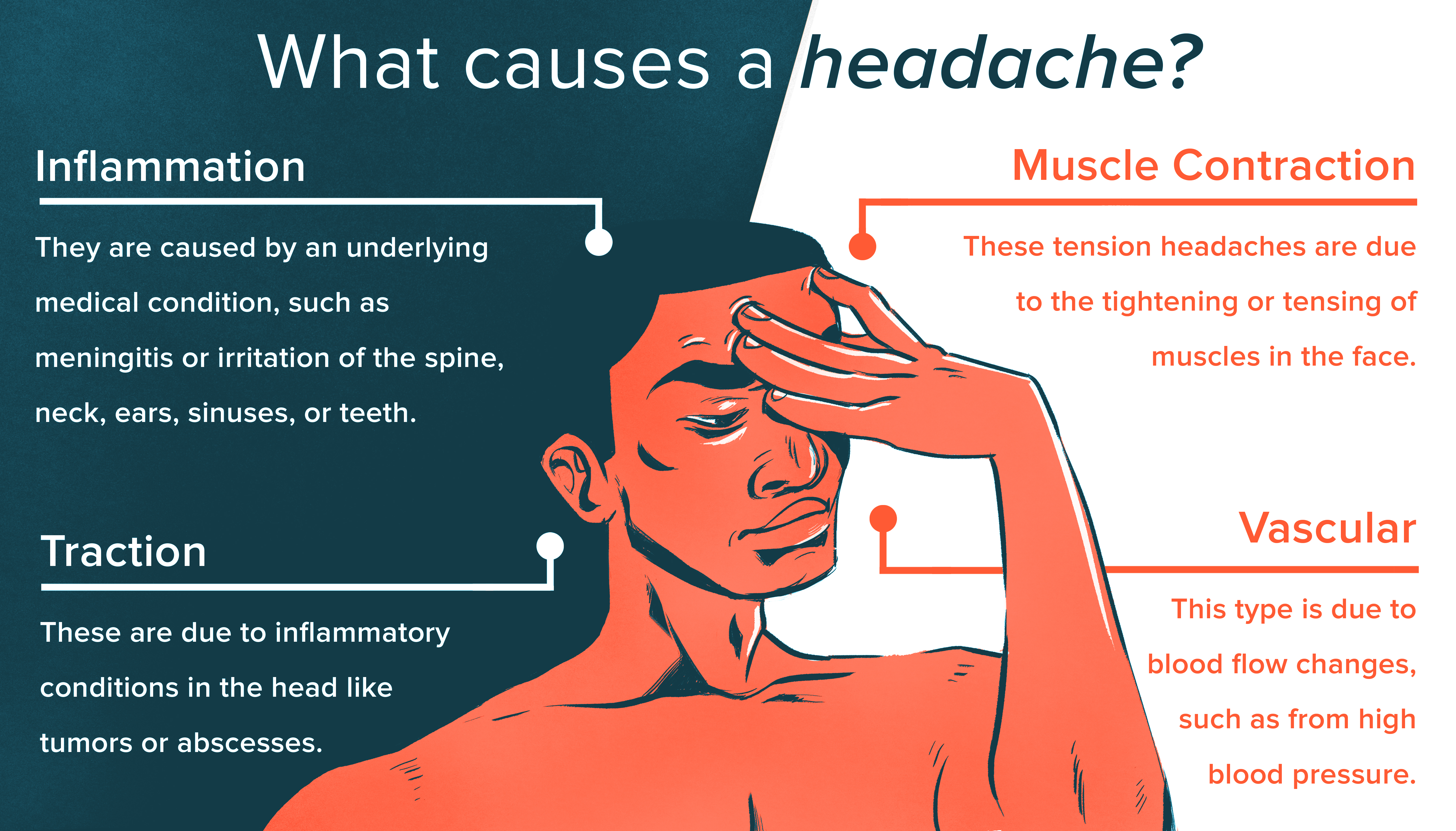
- Inflammation: The release of prostaglandins, hormone-like compounds involved in inflammation and pain, can be heightened during menstruation and contribute to headaches.
- Stress and tension: Menstruation can already be a stressful time for some women, and stress and tension can trigger headaches or make existing headaches worse.
- Dehydration: Fluid retention during the menstrual cycle can lead to dehydration, which is a known trigger for headaches.
It\'s essential for individuals experiencing migraines during menstruation to manage their symptoms effectively. Some strategies to consider include:
- Keeping track of menstrual cycles and potential triggers in a headache diary
- Maintaining a healthy lifestyle with regular exercise, sufficient sleep, and a balanced diet
- Managing stress through relaxation techniques, such as deep breathing exercises or meditation
- Staying hydrated by drinking enough water throughout the day
- Taking over-the-counter pain medications or consulting a healthcare professional for prescribed migraine medications
It\'s important to consult with a healthcare provider for personalized advice and to rule out any underlying medical conditions that could be contributing to the headaches during menstruation.
READ MORE:
Overview of Menstrual Headaches
Menstrual headaches, often experienced as part of premenstrual syndrome, are primarily linked to hormone fluctuations, particularly a drop in estrogen levels before menstruation. These headaches can range from mild to severe and are typically accompanied by other symptoms like bloating and cramping.
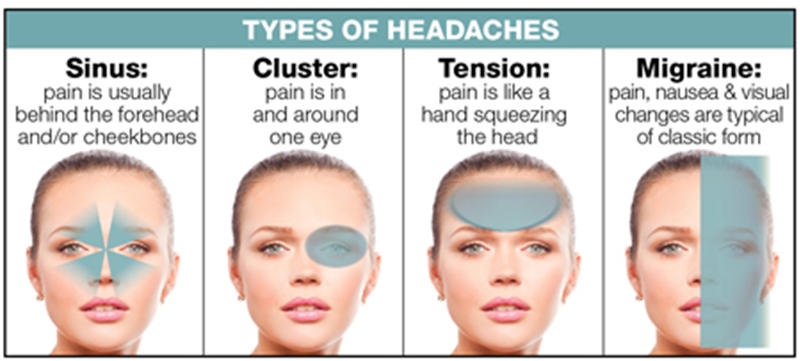
- Understanding Menstrual Migraines: These migraines usually begin two days before the period and can last until the third day. They"re characterized by intense throbbing or pulsing in one area of the head, nausea, vomiting, and sensitivity to light and sound. Unlike other migraines, menstrual migraines typically do not include an aura.
- Severity and Frequency: Menstrual migraines are often more severe, last longer, and are less responsive to treatment compared to other migraines. Most women experience migraines at various times of the month, but a small percentage have migraines only during menstruation.
- Hormonal Influences: The natural drop in estrogen and the increase in prostaglandin levels are key factors in triggering menstrual migraines. These hormonal changes can significantly impact headache patterns.
- Diagnosis: There are no specific tests for menstrual migraines. Keeping a migraine diary for at least three months, noting both migraine attacks and menstruation days, is the most accurate method for diagnosis.
- Treatment Approaches: Treatment options include non-steroidal anti-inflammatory drugs (NSAIDs), estrogen supplements, and triptans, depending on the regularity of the menstrual cycle and the need for contraception. Preventive measures might also involve combined hormonal contraceptives to stabilize estrogen levels and manage migraines.
It"s important to consult a healthcare professional if the quality, severity, or timing of menstrual headaches changes, as it could indicate other medical conditions, including the onset of perimenopause.

Hormonal Fluctuations and Their Impact
Hormonal changes are a significant factor in menstrual headaches, particularly the rapid drop in estrogen levels just before the menstrual cycle. This decrease in estrogen, coupled with the increase in prostaglandins (hormones produced in the uterus), can lead to the onset of headaches.
- Role of Estrogen: The natural decline in estrogen levels before menstruation is a primary trigger for menstrual migraines. Estrogen"s role in regulating various body functions, including pain perception, explains why its fluctuation can lead to headaches.
- Impact of Prostaglandins: Higher levels of prostaglandins during heavy and painful periods are also linked to the occurrence of menstrual migraines, indicating a significant hormonal influence on these headaches.
- Severity and Duration: Hormonal fluctuations can make menstrual migraines more severe, longer-lasting, and less responsive to typical migraine treatments compared to other types of headaches.
- Diagnosis and Monitoring: Since there are no specific tests for menstrual migraines, keeping a detailed diary of migraine attacks and menstruation can help in diagnosing and understanding the pattern of these headaches.
- Management Strategies: Understanding these hormonal changes can assist in developing effective treatment strategies, including hormonal contraceptives, which stabilize estrogen levels and help manage migraine attacks.
Understanding these hormonal dynamics is crucial in managing menstrual migraines, as they influence both the occurrence and severity of the headaches. Healthcare professionals often recommend tracking headache patterns in relation to the menstrual cycle to tailor treatment effectively.
Identifying Menstrual Migraines
Menstrual migraines, a specific type of migraine linked to the menstrual cycle, tend to be more severe, last longer, and are less responsive to treatment compared to other migraines. They are primarily identified by their timing and symptoms.
- Timing of the Migraine: These migraines typically start two days before the period and can last until the third day of menstruation. They are closely linked to the hormonal changes that occur during this time.
- Symptoms: Menstrual migraines are characterized by intense throbbing or pulsing in one area of the head. Accompanying symptoms include nausea, vomiting, and extreme sensitivity to light and sound. Unlike other migraines, they usually don"t have an aura.
- Diagnosis: There are no specific tests for menstrual migraines. The most accurate way to diagnose them is by keeping a detailed diary of migraine attacks and menstrual cycles for at least three months.
- Role of Estrogen and Prostaglandins: The drop in estrogen levels before menstruation and increased levels of prostaglandins are major triggers. Women with heavy and painful periods often experience higher levels of prostaglandin, which contributes to menstrual migraines.
- Treatment Considerations: Treatment can vary based on the regularity of menstrual cycles and other factors like the need for contraception. NSAIDs, estrogen supplements, and triptans are common treatments. Hormonal contraceptives can also help by stabilizing estrogen levels.
Understanding and identifying menstrual migraines is crucial for effective management and treatment. It involves recognizing the unique timing and symptoms of these migraines and working closely with a healthcare provider to find the most suitable treatment approach.

Lifestyle Factors and Triggers
Lifestyle factors and certain triggers can significantly influence the occurrence and severity of menstrual migraines. Being aware of these can help in managing and possibly reducing the frequency of these headaches.
- Hormonal Changes: Rapid changes in estrogen levels before the menstrual cycle are a primary trigger for menstrual migraines. Prostaglandins, hormones produced in the uterus, also play a role in triggering these headaches.
- Diet and Hydration: Certain foods and dehydration can trigger migraines. Maintaining a balanced diet and staying well-hydrated, especially during the menstrual cycle, can help in reducing migraine occurrences.
- Stress Management: Stress is a known trigger for migraines. Employing stress management techniques like meditation, yoga, or regular exercise can help in reducing the frequency of migraines.
- Sleep Patterns: Irregular sleep patterns can trigger migraines. Ensuring a regular sleep schedule and getting enough rest is crucial for migraine management.
- Journaling and Tracking: Keeping a migraine journal can be helpful in identifying specific triggers related to lifestyle, diet, or stress. This information can be invaluable for both you and your healthcare provider in managing menstrual migraines.
- Avoiding Known Triggers: Common triggers like bright lights, loud noises, or certain odors can exacerbate migraines. Identifying and avoiding these triggers can help in reducing the frequency and severity of migraines.
By understanding and managing these lifestyle factors and triggers, you can take proactive steps in reducing the impact of menstrual migraines on your daily life. Consulting with a healthcare professional can provide more personalized strategies based on your specific needs and triggers.
Effective Home Remedies
Managing menstrual migraines with home remedies can be an effective way to alleviate symptoms. These remedies focus on lifestyle adjustments and natural methods to reduce the severity and frequency of headaches.
- Hydration: Staying well-hydrated is crucial. Dehydration can trigger migraines, so drinking plenty of water, especially during the menstrual cycle, is important.
- Dietary Changes: Eating a balanced diet and avoiding known migraine triggers like chocolate, caffeine, and aged cheeses can help. Including magnesium-rich foods like leafy greens may also be beneficial.
- Regular Exercise: Regular physical activity, such as yoga or walking, can reduce stress and help manage migraine symptoms.
- Stress Reduction: Techniques like meditation, deep breathing exercises, and other relaxation techniques can help manage stress, which is a known migraine trigger.
- Adequate Sleep: Maintaining a regular sleep schedule and ensuring enough sleep can help prevent migraines.
- Cold Compress: Applying a cold compress to the forehead or neck can provide temporary pain relief.
- Essential Oils: Some people find relief using essential oils like peppermint or lavender oil, applied topically after dilution or used in aromatherapy.
- Herbal Remedies: Certain herbs, such as feverfew and butterbur, may help in preventing migraines. However, it"s important to consult with a healthcare provider before starting any herbal remedy.
While these home remedies can be effective, it"s important to remember that they are part of a larger management plan that includes understanding triggers and possibly consulting with a healthcare professional for severe or persistent migraines.
:max_bytes(150000):strip_icc()/what-is-a-menstrual-migraine-1719930_v2-3cca14811df0401fb429e9d738c53a5a-4f27a94438104586ad86fe57135d2d5d.png)
Medical Treatments and Pain Relief
Various medical treatments are available to help manage and relieve menstrual migraine pain. These treatments range from over-the-counter medications to prescription drugs and should be discussed with a healthcare provider for personalized care.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Commonly used NSAIDs for menstrual migraines include Ketoprofen, Ibuprofen, Fenoprofen calcium, Naproxen, and Nabumetone. These are often started two to three days before the period and continued through the menstrual flow.
- Triptans: These are selective serotonin receptor agonists used for acute migraines. Common triptans include Almotriptan, Eletriptan, Frovatriptan, Naratriptan, Rizatriptan, Sumatriptan, and Zolmitriptan. They are taken to stop menstrual migraines after they begin.
- Other Medications: Additional treatment options may include small doses of ergotamine or methylergonovine maleate, beta-blockers like propranolol, anticonvulsants such as topiramate, calcium channel blockers like verapamil, estrogen patches, gels, or pills, contraceptives, dihydroergotamines (DHE), caffeine, analgesics, and corticosteroids.
- Hormonal Contraceptives: Combined hormonal contraceptives can help in stabilizing estrogen levels and managing migraine headaches. They also offer additional benefits like regular menstrual cycles, acne treatment, and controlling heavy menstrual bleeding.
It"s important to consult with a healthcare provider to find the most suitable treatment option, especially for severe or persistent migraines. They can provide guidance based on individual health needs and migraine patterns.
How to alleviate headaches during menstruation
\"Are you tired of experiencing unbearable menstrual headaches every month? Discover the ultimate solution to relieve your pain and make your life more enjoyable. Watch this video now and say goodbye to menstrual headaches forever!\"
Understanding menstrual migraines: causes and solutions
\"Suffering from debilitating menstrual migraines that disrupt your daily routine? Don\'t fret anymore! Discover the most effective techniques to manage and prevent menstrual migraines. Click to watch this video and reclaim your life!\"
When to Consult a Healthcare Professional
Knowing when to seek medical advice for menstrual migraines is important for effective management and treatment. Here are some situations where consulting a healthcare professional is recommended:
- Severe or Unusual Symptoms: If your headaches are unusually severe, last longer than usual, or have symptoms that are different from your typical menstrual migraines, it"s important to seek medical advice.
- Lack of Response to Over-the-Counter Medications: If over-the-counter pain medications do not provide relief, a healthcare professional can prescribe stronger medications or suggest alternative treatments.
- Changes in Headache Patterns: Any significant change in the frequency, severity, or timing of your headaches could indicate an underlying medical issue. This is particularly important as it could signal the onset of perimenopause, which can affect headache patterns.
- Considering Hormonal Contraceptives: For those considering hormonal contraceptives to manage migraines, a healthcare provider can advise on the best option, especially since certain forms, like combined hormonal contraceptives, are not recommended for people with migraines with aura due to increased stroke risk.
- Other Health Concerns: If you have other risk factors for stroke or health concerns, professional guidance is crucial in choosing the right form of contraception or treatment for migraines.
It"s always advisable to keep a detailed migraine diary and discuss it with your healthcare provider for personalized management and treatment strategies.

READ MORE:
Preventive Strategies and Lifestyle Modifications
Preventing menstrual migraines involves a combination of lifestyle changes and strategies. These modifications can help in reducing the frequency and severity of migraines associated with your menstrual cycle.
- Understanding Hormonal Changes: Recognize the role of hormonal fluctuations, especially the drop in estrogen before your period, which can trigger migraines. Being aware of these changes can help in planning and managing symptoms.
- Maintaining a Migraine Diary: Keep a detailed diary of your migraine attacks and menstrual cycle. This can help in identifying patterns and triggers, and is useful for discussions with your healthcare provider.
- Regular Medication Regimen: If prescribed by a doctor, certain medications like NSAIDs or triptans can be taken a few days before the expected start of your period and continued until a few days after it begins, to help prevent migraines.
- Contraceptive Choices: Discuss contraceptive options with your healthcare provider. Certain contraceptives can help manage menstrual migraines by stabilizing hormone levels, but the choice of contraceptive should be made considering individual health conditions, especially if you experience migraine with aura.
- Lifestyle Adjustments: Simple changes like maintaining a healthy diet, regular exercise, adequate sleep, and stress management can significantly impact the frequency and severity of migraines.
- Avoiding Known Triggers: Identifying and avoiding personal migraine triggers, such as certain foods, dehydration, or stress, can be an effective prevention strategy.
Implementing these strategies requires consistency and may involve trial and error to identify what works best for you. Consultation with a healthcare professional is essential for personalized advice and treatment.
Understanding the causes and remedies for menstrual migraines can empower you to manage these headaches effectively. Remember, with the right strategies and medical guidance, you can significantly alleviate discomfort and improve your quality of life.





:max_bytes(150000):strip_icc()/VWH_Illustration_Natural-Remedies-for-Managing-Headaches_Paige-McLaughlin_Final-461a780622884c479edf3dc01234692c.jpg)


:max_bytes(150000):strip_icc()/VWH_Illustration_Getting-Rid-of-a-Migraine_Illustrator_Ellen-Lindner_Final-a245985cbf4645a7874d573991fb6cbb.jpg)