Topic how to make period headaches go away: Discover effective and empowering ways to alleviate period headaches in our comprehensive guide, "How to Make Period Headaches Go Away", offering practical advice and insights for lasting relief.
Table of Content
- How to make period headaches go away?
- Understanding Period Headaches and Menstrual Migraines
- Self-Care and Lifestyle Changes for Migraine Relief
- The Role of Magnesium in Migraine Prevention
- Effective Exercise Routines for Reducing Migraine Frequency
- Medical Treatments: NSAIDs and Triptans
- Alternative Remedies: Acupressure and CBD
- YOUTUBE: Are headaches during menstruation normal? - Dr. Manjit Matharu
- The Impact of Birth Control on Menstrual Migraines
- Prescription Medications for Direct Migraine Treatment
How to make period headaches go away?
To make period headaches go away, you can follow these steps:
- Ensure you are getting enough sleep and maintain a regular sleep schedule, waking up and going to bed at around the same times every day.
- Eat regular meals and avoid skipping any. Try to include protein in your diet.
- Keep your blood sugar levels stable by eating small, frequent snacks throughout the day.
- Apply a cold or hot compress to your head or neck to help relieve pain.
- Try relaxation techniques such as deep breathing, meditation, or yoga to reduce stress.
- Consider over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen to alleviate symptoms.
- Consult with your healthcare provider to explore other options for hormonal headache treatments.
READ MORE:
Understanding Period Headaches and Menstrual Migraines
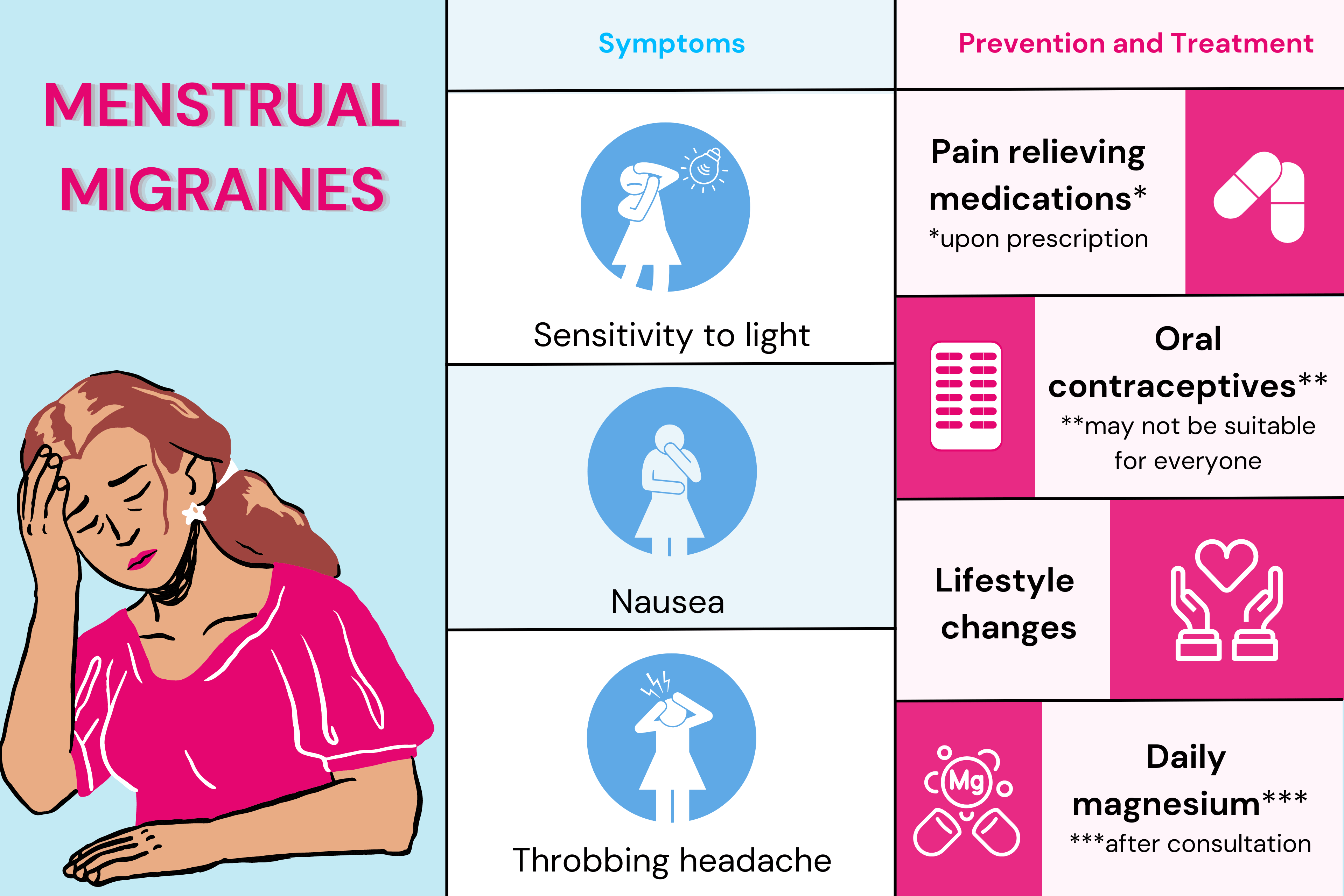
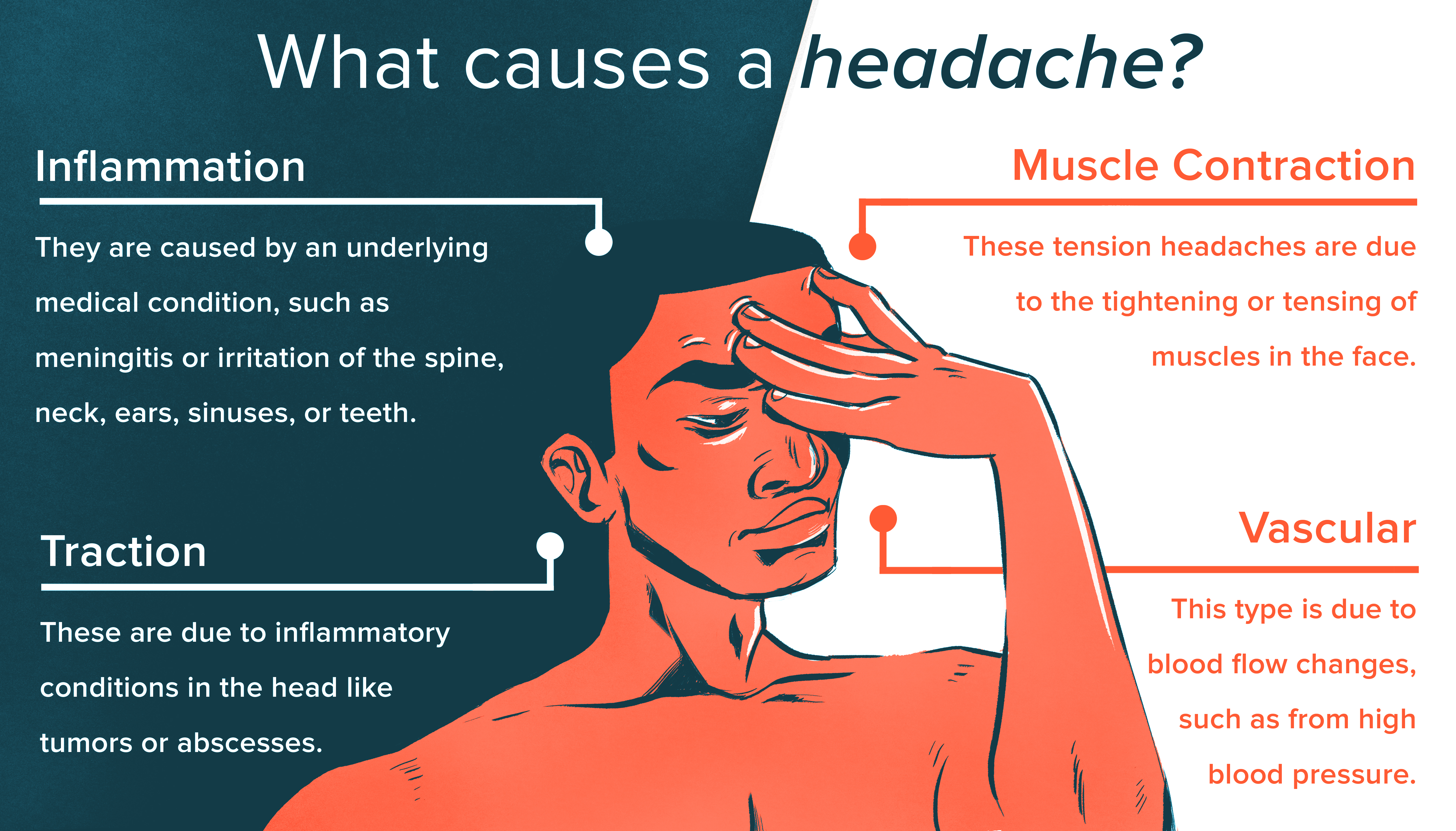
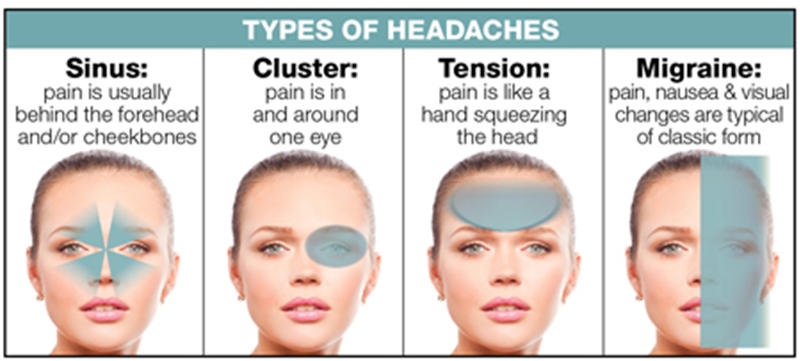
Period headaches, often manifesting as menstrual migraines, are primarily influenced by hormonal fluctuations in the body. A drop in estrogen levels before or during menstruation is a common trigger for these headaches. Understanding their nature is crucial for effective management and treatment.
- Self-Care and Lifestyle: Regular sleep patterns, balanced diet including protein-rich meals, and consistent aerobic exercise play a significant role in reducing the frequency and severity of migraine attacks.
- Magnesium Supplements: Daily magnesium intake has been shown to have a preventive effect on menstrual migraines. However, it"s important to consult with a healthcare provider before starting any supplements.
- Medical Treatments: Nonsteroidal anti-inflammatory medications (NSAIDs) and triptans are commonly used for managing menstrual migraines. These medications should ideally be started a few days before the onset of menstruation and continued through the menstrual flow.
- Alternative Approaches: Techniques like acupressure may offer relief from migraine symptoms, though clinical evidence is limited. It"s a non-invasive and cost-free method that can be self-administered.
- Hormonal Control: Birth control methods can stabilize hormone levels, potentially reducing the occurrence of menstrual migraines. However, those who experience migraine with aura should exercise caution with estrogen-containing birth control.
- Prescription Medications: In addition to NSAIDs and triptans, anticonvulsants, antidepressants, and beta-blockers can also be prescribed to manage and prevent migraines.
It"s essential to keep a migraine journal to track symptoms, duration, and triggers. This information can be valuable for healthcare providers to tailor a treatment plan that"s most effective for your specific condition.

Self-Care and Lifestyle Changes for Migraine Relief
Effective management of period headaches often involves self-care and lifestyle adjustments. Understanding these changes and incorporating them into your daily routine can significantly alleviate migraine symptoms.
- Maintain a Regular Sleep Schedule: Aim for consistent sleep times to help regulate your body"s natural rhythms. Adequate sleep is crucial in managing migraines.
- Engage in Regular Exercise: Activities like aerobic exercise, yoga, and high-intensity interval training (HIIT) have been found to reduce migraine frequency and intensity.
- Stay Hydrated: Drink water and other hydrating fluids regularly to prevent headaches caused by dehydration.
- Healthy Diet: Eating balanced meals rich in fruits, vegetables, lean protein, and whole grains can help. Avoid potential headache triggers like caffeine, alcohol, and processed foods.
- Stress Management: Practice relaxation techniques such as deep breathing, meditation, or yoga to manage stress effectively.
- Consider Magnesium Supplements: Daily magnesium intake may prevent menstrual migraines. Consult with a healthcare provider before starting any supplement regimen.
- Use Essential Oils: Oils like lavender, peppermint, and eucalyptus can be applied to temples or neck for relief. Always dilute with a carrier oil for safety.
- Try Acupressure: Acupressure involves applying pressure to specific body points and can be effective in relieving pain and tension.
Remember, these are general guidelines and it"s important to consult a healthcare professional for personalized advice. Adapting these self-care practices can significantly improve your quality of life during menstrual cycles.
The Role of Magnesium in Migraine Prevention
Magnesium plays a vital role in preventing menstrual migraines. It is known for its potential benefits in stabilizing cellular functions and reducing neuronal hyperexcitability, which are key factors in migraine development.
- How Magnesium Helps: While the exact mechanisms are still being studied, magnesium is believed to help prevent menstrual migraines by stabilizing cellular activity and reducing brain neuron excitability.
- Evidence Supporting Magnesium: Several studies, including clinical trials, have suggested that daily magnesium supplements can be effective in reducing migraine frequency, especially in those with premenstrual migraines.
- Recommended Forms of Magnesium: Magnesium citrate, among other types, is often recommended for migraine prevention. It"s available over the counter, but it"s always wise to consult a healthcare provider before starting any supplement.
- Integrating Magnesium into Your Routine: Regular intake of magnesium supplements as part of your daily routine could help in reducing the incidence of menstrual migraines.
- Consultation with Healthcare Providers: Always discuss with a healthcare provider before beginning any new supplement regimen, particularly to ensure it doesn"t interfere with other medications or conditions.
Incorporating magnesium supplements, as advised by a healthcare professional, can be a safe and cost-effective strategy for many in managing and preventing menstrual migraines.
Effective Exercise Routines for Reducing Migraine Frequency
Regular exercise is a key strategy in reducing the frequency and severity of menstrual migraines. Incorporating certain types of physical activity into your routine can have a significant impact on your overall well-being and migraine management.
- Aerobic Exercise: Engaging in daily aerobic exercise for about 20 to 30 minutes can be highly beneficial. Activities such as brisk walking, jogging, cycling, or swimming are excellent choices.
- Yoga: Yoga practices, known for promoting relaxation and stress reduction, can also help in managing migraines. Certain yoga poses are particularly effective in releasing tension that can trigger migraines.
- High-Intensity Interval Training (HIIT): HIIT, which involves short bursts of intense exercise followed by rest periods, can also be effective. It"s important to start slowly and increase intensity gradually.
- Consistency is Key: Regularity in exercise is crucial. Try to incorporate physical activity into your daily routine to maintain consistency.
- Listen to Your Body: Always be mindful of how your body responds to different exercises and adjust your routine accordingly. It"s important not to overexert yourself, especially during a migraine.
Remember, while exercise can be a powerful tool in managing migraines, it"s important to consult with a healthcare professional before starting any new exercise regimen, especially if you have specific health concerns or conditions.
Medical Treatments: NSAIDs and Triptans
For menstrual migraine relief, medical treatments such as Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and Triptans are commonly prescribed. These medications play a crucial role in both alleviating pain during a migraine attack and in some cases, preventing their onset.
- NSAIDs: These include medications like Ibuprofen, Naproxen, and Ketoprofen. They are often effective in reducing the inflammation and pain associated with menstrual migraines. Starting NSAID treatment a few days before the onset of your period can be beneficial.
- Triptans: Triptans are specifically targeted towards treating migraines. They work by constricting blood vessels and blocking pain pathways in the brain. Triptans are generally used at the onset of migraine symptoms.
- Types of Triptans: There are several types of triptans, such as Sumatriptan, Rizatriptan, and Zolmitriptan, each with its own specific usage instructions.
- Considerations: While these medications are effective, it"s important to discuss potential side effects and contraindications with your healthcare provider, especially if you have other medical conditions or are taking other medications.
- Personalized Treatment: The effectiveness of these treatments can vary from person to person. Keeping a migraine journal can be helpful in tracking the effectiveness of these medications for your specific case.
Always consult with a healthcare professional before starting any new medication to ensure it"s appropriate for your particular health situation.
:max_bytes(150000):strip_icc()/what-is-a-menstrual-migraine-1719930_v2-3cca14811df0401fb429e9d738c53a5a-4f27a94438104586ad86fe57135d2d5d.png)
Alternative Remedies: Acupressure and CBD
When considering alternative remedies for menstrual migraines, acupressure and CBD (Cannabidiol) have gained attention for their potential benefits. These natural methods can provide relief for some people, offering a complementary approach to traditional medical treatments.
- Acupressure: This technique involves applying pressure to specific points on the body to relieve pain. While clinical evidence is limited, anecdotal experiences suggest it can help with pain, nausea, anxiety, and depression that accompany migraines.
- How to Use Acupressure: Acupressure can be self-administered, focusing on key points known to alleviate headache symptoms. It"s a non-invasive, cost-free approach that can be tried alongside other treatments.
- CBD: CBD has been explored for its potential in treating migraine-related symptoms, particularly nausea. However, it"s important to be aware of local laws and the quality of CBD products, as they vary widely.
- Using CBD: If considering CBD, research its efficacy and safety, and consult with a healthcare professional, especially regarding interactions with other medications.
These alternative remedies can be part of a broader approach to managing menstrual migraines, especially for those looking for natural methods. As with any treatment, it"s advisable to consult with a healthcare provider to determine what"s best for your individual needs.
Are headaches during menstruation normal? - Dr. Manjit Matharu
Discover the power of understanding your menstrual cycle and how it affects your body in this enlightening video. Learn valuable tips and tricks to navigate through menstruation with ease and embrace this natural process.
Managing Menstrual Migraines and Hormonal Headaches
Say goodbye to debilitating migraines with this informative video that uncovers effective strategies to prevent and alleviate these intense headaches. Gain insights on how to identify triggers and adopt lifestyle changes for a headache-free life.
The Impact of Birth Control on Menstrual Migraines
Birth control plays a significant role in managing menstrual migraines for many women. It works by stabilizing hormonal fluctuations, which are a common trigger for these migraines.
- Hormonal Regulation: Birth control helps in regulating hormones, especially estrogen levels, which can significantly reduce the frequency of menstrual migraines.
- Types of Birth Control: Various forms of birth control, including pills, patches, and injections, can be effective. It"s important to choose the right type based on individual health needs and migraine patterns.
- Considerations for Migraine with Aura: Women who experience migraine with aura need to be cautious about using birth control containing estrogen due to an increased risk of stroke. Alternatives like progestin-only options might be safer.
- Consultation with Healthcare Providers: Discussing your migraine history and any associated risks with a healthcare provider is crucial in determining the most suitable birth control method for migraine management.
- Personalized Approach: The effectiveness of birth control in managing menstrual migraines can vary from person to person, making personalized medical advice essential.
While birth control can be an effective strategy for some, it"s important to consider individual health factors and consult with a healthcare professional to determine the best approach for managing menstrual migraines.

READ MORE:
Prescription Medications for Direct Migraine Treatment
Prescription medications play a critical role in the direct treatment of menstrual migraines. They are designed to alleviate symptoms during an attack and, in some cases, help in preventing their onset.
- Triptans: Triptans are often the go-to prescription medication for acute migraine attacks. They work by constricting blood vessels in the brain and blocking pain pathways. There are several types, including Sumatriptan, Rizatriptan, and Zolmitriptan, each with specific instructions for use.
- NSAIDs: Nonsteroidal anti-inflammatory drugs such as Ibuprofen and Naproxen are also used in treating menstrual migraines, especially for pain relief. They can be taken a few days before the period starts and continued through the menstrual flow.
- Other Medications: Depending on the individual"s specific needs and migraine patterns, healthcare providers might also prescribe medications like anticonvulsants, antidepressants, beta blockers, and calcium channel blockers.
- Personalized Treatment: It"s important to consult with a healthcare provider to determine the most suitable medication based on individual health conditions and migraine patterns.
- Monitoring Side Effects: Be aware of the potential side effects of these medications and communicate any concerns with your healthcare provider for appropriate management.
Effective management of menstrual migraines often requires a combination of the right prescription medications and lifestyle adjustments. Always consult with a healthcare professional for a tailored treatment plan.
Conquering period headaches is possible with a blend of self-care, lifestyle changes, and medical treatments. Explore these strategies to find relief and take control of your menstrual health, enhancing your overall well-being.





:max_bytes(150000):strip_icc()/VWH_Illustration_Natural-Remedies-for-Managing-Headaches_Paige-McLaughlin_Final-461a780622884c479edf3dc01234692c.jpg)

