Topic headache on top of head: Experiencing a headache on top of your head can be troubling, but understanding its causes and finding effective relief is entirely possible. Discover strategies to alleviate discomfort and improve your well-being.
Table of Content
- What are the causes of a headache on top of the head?
- Common Causes of Headache on Top of Head
- Symptoms Associated with Top of Head Headaches
- When to See a Doctor for Headaches on Top of Head
- Diagnosis Processes for Top of Head Headaches
- Effective Treatments for Headache on Top of Head
- Home Remedies and Lifestyle Changes for Managing Headaches
- YOUTUBE: How to Relieve Vertex Headache - Check This Muscle
- Preventive Measures to Avoid Headaches on Top of Head
- Understanding Tension Headaches vs. Migraines
- Impact of Dehydration and Diet on Headaches
- The Role of Stress Management in Preventing Headaches
What are the causes of a headache on top of the head?
A headache on top of the head can be caused by various factors including:
- Tension headaches: These are the most common type of headache and are often described as a dull, aching pain that feels like a tight band around the head. Tension headaches can be caused by stress, poor posture, eye strain, or muscle tension in the neck and scalp.
- Migraines: Migraines are intense headaches that are often accompanied by symptoms such as nausea, vomiting, sensitivity to light and sound, and visual disturbances. Migraines can affect any part of the head, including the top.
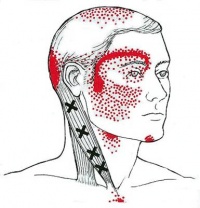
- Occipital neuralgia: This condition is characterized by sharp, shooting pain that radiates from the base of the skull to the top of the head. It is caused by irritation or inflammation of the occipital nerves, which run from the top of the spinal cord up to the scalp.
Other potential causes of a headache on top of the head include sinusitis, high blood pressure, head injuries, and certain medications. It is important to consult a healthcare professional to determine the underlying cause of your headache and to receive appropriate treatment.
READ MORE:
Common Causes of Headache on Top of Head
Headaches on the top of the head can be caused by various factors, each with its own approach to management and treatment. Understanding these causes can help in identifying the best relief methods.
- Tension Headaches: Often resulting from stress, poor posture, or muscle strain, leading to a dull, aching sensation across the top of the head.
- Migraine: Migraines can cause intense pain on one or both sides of the head, sometimes affecting the top. Sensitivity to light, noise, or smells may accompany the pain.
- Cluster Headaches: These are severe, recurrent headaches that can cause a piercing pain on one side of the head, sometimes extending to the top.
- Dehydration: Lack of adequate hydration can lead to a headache on the top of the head, emphasizing the importance of regular water intake.
- Sinusitis: Infection or inflammation of the sinus can cause pressure and pain on the top of the head, among other areas.
- Occipital Neuralgia: A condition where the occipital nerves are inflamed or injured, causing sharp, severe pain on the top of the head and back of the neck.
Each of these conditions may require a different approach to relief and management, highlighting the importance of proper diagnosis and treatment planning.

Symptoms Associated with Top of Head Headaches
Understanding the symptoms that accompany headaches on the top of the head can be crucial for identifying the underlying cause and seeking appropriate treatment.
- Dull, Aching Pain: A common symptom, presenting as a constant, dull pressure on the top of the head.
- Sharp, Stabbing Pain: Some individuals may experience sudden, sharp pains that feel like stabbing sensations on the top of their head.
- Sensitivity to Light and Sound: Often accompanying migraines, this sensitivity can exacerbate the discomfort of a headache.
- Nausea and Vomiting: Severe headaches, particularly migraines, may lead to feelings of nausea or even cause vomiting.
- Tenderness in Scalp: The area on the top of the head may feel tender to the touch, a symptom that can accompany tension headaches.
- Visual Disturbances: Some headache disorders, like migraines, can cause visual symptoms such as flashing lights or blind spots.
- Neck Pain: Tension in the neck muscles can lead to headaches on the top of the head, often accompanied by neck pain or stiffness.
Recognizing these symptoms is a step towards effective management, guiding individuals to seek the right treatment and relief strategies.
When to See a Doctor for Headaches on Top of Head
While many headaches can be managed with at-home treatments, certain signs warrant professional medical advice to prevent complications and address underlying causes.
- Sudden Onset: A headache that starts abruptly and is severe in nature, often described as a "thunderclap" headache, requires immediate medical attention.
- Increasing Frequency or Severity: Headaches that become more frequent or severe over time should be evaluated by a healthcare provider.
- Change in Headache Pattern: Any significant change in the characteristics of your headaches, including new symptoms, should prompt a doctor"s visit.
- Accompanied by Other Symptoms: Headaches with fever, stiff neck, confusion, seizures, double vision, weakness, numbness, or difficulty speaking are concerning and require prompt medical evaluation.
- Impact on Daily Life: If headaches start to affect your ability to perform daily tasks or significantly impact your quality of life, seek medical advice.
- Not Responding to Medication: Headaches that do not improve with over-the-counter medication warrant a consultation with a healthcare professional.
- After a Head Injury: Headaches that develop after a head injury, especially if they worsen, may indicate a concussion or other serious condition.
Seeking medical advice in these situations can help ensure proper diagnosis and treatment, reducing the risk of complications and improving quality of life.

Diagnosis Processes for Top of Head Headaches
Accurate diagnosis is crucial for effective treatment of headaches on the top of the head. Medical professionals use a variety of methods to diagnose the cause of these headaches.
- Patient History: The first step involves a detailed discussion about the headaches, including their onset, duration, frequency, and characteristics of the pain, as well as any associated symptoms or triggers.
- Physical Examination: A comprehensive physical exam, focusing on the head and neck, to identify any physical factors contributing to the headaches.
- Neurological Examination: To check for any neurological abnormalities that might be associated with the headaches, including reflexes, muscle strength, eye movements, and sensory function.
- Imaging Tests: In some cases, imaging tests such as MRI or CT scans may be recommended to rule out structural causes of the headache, such as tumors or sinus issues.
- Blood Tests: Blood tests can help identify any underlying conditions that might be causing the headaches, such as infections or thyroid problems.
- Referral to Specialists: Depending on the findings, you may be referred to a specialist, such as a neurologist, for further evaluation and treatment.
These diagnostic steps help healthcare providers determine the underlying cause of the headache on top of the head and develop an effective treatment plan tailored to the individual"s specific needs.
Effective Treatments for Headache on Top of Head
Finding relief from headaches on the top of the head involves a combination of treatments tailored to the individual"s condition and the underlying cause. Here are some effective strategies:
- Medication: Over-the-counter pain relievers like ibuprofen, acetaminophen, or aspirin can be effective for mild to moderate headaches. For more severe headaches, prescription medications, including triptans for migraines, may be necessary.
- Stress Management: Since stress can be a significant trigger for headaches, techniques such as meditation, yoga, and deep-breathing exercises can be beneficial in reducing their frequency and severity.
- Physical Therapy: For headaches caused by muscle tension or postural issues, physical therapy can help relieve pain through exercises that strengthen and stretch the neck and back muscles.
- Lifestyle Changes: Regular exercise, maintaining a healthy diet, staying hydrated, and ensuring sufficient sleep can help reduce the occurrence of headaches.
- Hydration: Drinking adequate amounts of water throughout the day is crucial, especially if dehydration is a trigger for your headaches.
- Avoiding Triggers: Identifying and avoiding personal headache triggers, such as certain foods, drinks, or environmental factors, can be an effective strategy for prevention.
- Acupuncture: Some people find relief from headache pain through acupuncture, a practice that involves inserting thin needles into specific points on the body.
- Massage: Massage therapy can help to reduce tension in the muscles of the head, neck, and shoulders, providing relief from headache pain.
Consultation with a healthcare provider can help determine the most appropriate treatment options based on the type and cause of your headache.

Home Remedies and Lifestyle Changes for Managing Headaches
Many headaches can be effectively managed with simple home remedies and adjustments to your lifestyle. These strategies can help alleviate symptoms and reduce the frequency of headaches.
- Adequate Hydration: Drinking enough water throughout the day can prevent headaches caused by dehydration.
- Regular Sleep Patterns: Maintaining a consistent sleep schedule helps prevent headaches by ensuring adequate rest and reducing stress.
- Stress Reduction Techniques: Activities such as yoga, meditation, and deep-breathing exercises can decrease stress levels, a common trigger for headaches.
- Limiting Caffeine and Alcohol: Reducing the intake of substances that can trigger headaches, such as caffeine and alcohol, can be beneficial.
- Healthy Diet: Eating balanced meals at regular intervals helps maintain stable blood sugar levels, reducing the risk of headache.
- Exercise: Regular physical activity can reduce the frequency and severity of headaches by improving overall health and reducing stress.
- Warm Compresses: Applying a warm compress to the neck and shoulders can help relax tense muscles, potentially relieving headache pain.
- Essential Oils: Inhaling or applying diluted essential oils like peppermint or lavender can provide relief from headache symptoms for some people.
- Limit Screen Time: Reducing exposure to screens, especially before bedtime, can help prevent headaches related to eye strain.
- Proper Posture: Maintaining good posture, especially while sitting for long periods, can prevent headaches caused by neck and shoulder strain.
Integrating these home remedies and lifestyle changes into your routine can offer significant relief from headaches and improve your overall well-being.
How to Relieve Vertex Headache - Check This Muscle
If you\'re tired of constantly battling muscle headaches, this video is a must-watch! Discover effective strategies and remedies to alleviate these nagging pains and reclaim your peace of mind. Don\'t let headaches hold you back any longer!
What Causes Headaches on Top of Head? - Top Health FAQ Channel
Looking for answers to your burning health questions? Look no further than the Top Health FAQ Channel! This informative video series covers a wide range of topics, from nutrition and fitness to mental well-being. Join the millions of viewers who have found valuable insights and helpful guidance here!
Preventive Measures to Avoid Headaches on Top of Head
Implementing preventive measures can significantly reduce the risk of experiencing headaches on top of the head. These strategies focus on lifestyle adjustments and healthy habits to minimize headache triggers.
- Maintain a Healthy Diet: Eat balanced meals at regular intervals to prevent low blood sugar levels, which can trigger headaches.
- Stay Hydrated: Drink adequate amounts of water throughout the day to avoid dehydration-related headaches.
- Regular Exercise: Engage in regular physical activity to reduce stress and improve overall health, which can in turn reduce the frequency of headaches.
- Adequate Sleep: Ensure you get enough sleep each night and maintain a consistent sleep schedule to prevent headaches.
- Stress Management: Incorporate stress-reduction techniques such as yoga, meditation, or deep-breathing exercises into your routine.
- Avoid Known Triggers: Identify and avoid personal headache triggers, which can include certain foods, beverages, or environmental factors.
- Limit Caffeine and Alcohol: Reduce your intake of caffeine and alcohol, as they can trigger headaches in some individuals.
- Good Posture: Practice good posture, especially if you spend long hours sitting, to prevent tension headaches caused by neck and shoulder strain.
- Screen Time Management: Take regular breaks from screens to avoid eye strain and headaches related to prolonged use of electronic devices.
- Regular Eye Checkups: Ensure your vision prescription is up to date and wear glasses if needed to avoid headaches caused by eye strain.
Adopting these preventive measures can help manage and reduce the occurrence of headaches on top of the head, leading to improved quality of life.

Understanding Tension Headaches vs. Migraines
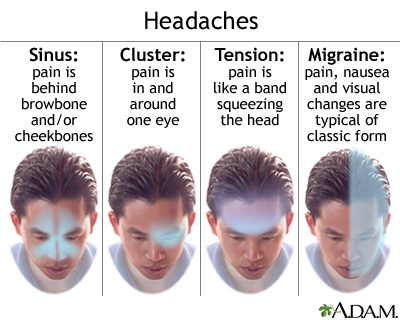
Knowing the difference between tension headaches and migraines is crucial for effective treatment and management. While both can cause pain on top of the head, they have distinct characteristics and triggers.
- Symptoms:
- Tension Headaches: Typically cause a dull, aching pain across the forehead or back of the head. They are often described as feeling like a tight band around the head.
- Migraines: Characterized by a pulsating, throbbing pain on one side of the head, but can also affect the top. Symptoms may include nausea, vomiting, and sensitivity to light and sound.
- Duration:
- Tension Headaches: Can last from 30 minutes to several days.
- Migraines: Typically last from 4 hours to 3 days.
- Triggers:
- Tension Headaches: Often triggered by stress, anxiety, poor posture, and lack of sleep.
- Migraines: Can be triggered by a wider range of factors, including hormonal changes, certain foods and drinks, weather changes, and sensory stimuli.
- Treatment:
- Tension Headaches: Usually managed with over-the-counter pain relievers, stress management, and lifestyle changes.
- Migraines: May require specific migraine medications, preventive treatments, and avoiding known triggers.
Understanding these differences helps in seeking appropriate care and adopting strategies to manage or prevent headaches effectively.
Impact of Dehydration and Diet on Headaches
The relationship between hydration, diet, and headaches is significant, with both playing a crucial role in the prevention and management of headache symptoms.
- Dehydration:
- Dehydration can lead to the development of headaches by causing the brain to temporarily contract or shrink from fluid loss. This mechanism triggers pain receptors surrounding the brain, leading to a dehydration headache.
- Staying hydrated is essential for preventing headaches. It is recommended to drink at least 8 glasses of water per day, more if you are active or in a hot climate.
- Diet:
- Certain foods and drinks can trigger headaches in susceptible individuals. Common culprits include aged cheeses, processed foods, red wine, chocolate, and foods containing MSG or artificial sweeteners.
- Maintaining a balanced diet with regular meal times can help prevent headaches. Incorporating fresh fruits, vegetables, lean proteins, and whole grains while avoiding known triggers is beneficial.
- Some individuals may find relief from headaches by following a diet low in tyramine or histamine, substances found in certain foods that can trigger headaches.
- Nutritional Deficiencies: Deficiencies in certain vitamins and minerals, such as magnesium, vitamin D, and B vitamins, have been linked to headaches. Ensuring a diet rich in these nutrients can help in headache prevention.
Understanding how dehydration and diet affect headaches can guide individuals in making lifestyle choices that reduce the frequency and severity of headaches.

READ MORE:
The Role of Stress Management in Preventing Headaches
Stress is a well-known trigger for headaches, including those on the top of the head. Managing stress effectively can significantly reduce the frequency and severity of headaches.
- Relaxation Techniques: Practices such as deep breathing, meditation, and progressive muscle relaxation can help lower stress levels and reduce the likelihood of stress-induced headaches.
- Regular Exercise: Physical activity is a powerful stress reliever. Activities like walking, swimming, or yoga can help manage stress and reduce headache occurrence.
- Adequate Sleep: Lack of sleep can exacerbate stress and lead to headaches. Ensuring 7-9 hours of quality sleep each night is crucial for stress management and headache prevention.
- Time Management: Overcommitment and poor time management can increase stress levels. Learning to prioritize tasks and say no when necessary can help manage stress.
- Healthy Lifestyle Choices: Eating a balanced diet, staying hydrated, and avoiding excessive caffeine and alcohol can help maintain optimal health and reduce stress.
- Seeking Support: Talking with friends, family, or a professional can provide emotional support and strategies for managing stress more effectively.
- Mindfulness and Cognitive Behavioral Therapy (CBT): These approaches can help change the perception of stress and improve coping mechanisms, reducing the impact of stress on headaches.
By incorporating stress management techniques into daily life, individuals can significantly reduce the risk of headaches and improve overall well-being.
Understanding the causes and effective management strategies for headaches on top of the head can empower you to lead a healthier, more comfortable life. Embrace these insights for relief and well-being.
:max_bytes(150000):strip_icc()/vision-and-headache-3422017_final-f90b31917b244236a7424b143a537fd3.jpg)
:max_bytes(150000):strip_icc()/migraine-relief-pressure-points-5205811-FINAL-cdc9e0d051cb460bac8baa98bc01954f.jpg)


:max_bytes(150000):strip_icc()/VWH-PaigeMcLaughlin-WhatisaClusterHeadache-Standard-87c962b6a28d4b1ab0359ed3ae5b696f.jpg)