Topic headache location meaning: Discover the "Headache Location Meaning" and unlock insights into your health. Learn how different headache locations can indicate various underlying conditions, guiding you towards better management and prevention strategies.
Table of Content
- What are the common reasons for experiencing headaches on one side of the head?
- Overview of Headache Types Based on Location
- Frontal Headaches: Tension and Sinus Related Causes
- Headaches in the Temporal Area: Migraine and Hormonal Influences
- Occipital Headaches: Cervicogenic and Occipital Neuralgia
- Headaches Behind the Eyes: Cluster Headaches and Sinus Issues
- Headaches Affecting the Entire Head: Dehydration and High Blood Pressure
- YOUTUBE: Understanding the Meaning of Headache Location
- Understanding Cluster Headaches: Symptoms and Treatments
- Neck-Originated Headaches: Cervicogenic Headaches and Treatment Options
- When to Seek Medical Attention for Your Headache
What are the common reasons for experiencing headaches on one side of the head?
When experiencing headaches on one side of the head, there are several common reasons that can be considered:
- Migraine: This type of headache often causes throbbing pain or a pulsing sensation primarily on one side of the head. Migraine attacks can last for hours or even days.
- Tension headache: Although typically felt on both sides of the head, tension headaches can sometimes be localized to one side. They are usually described as a band-like pressure or tightness around the head.
- Cluster headache: These headaches are intense and occur in clusters or cycles, usually on one side of the head. They often come with other symptoms such as eye redness, tearing, or stuffy nose.
- Sinus headache: Inflammation or infection of the sinuses can lead to localized pain in the head, often on one side. Sinus headaches are typically accompanied by facial pressure or congestion.
- Hemicrania continua: This rare type of headache is characterized by continuous pain on one side of the head. It is often accompanied by autonomic symptoms like tearing, nasal congestion, or drooping eyelid.
It\'s important to consult with a healthcare professional for a proper diagnosis and to determine the most appropriate treatment for your specific case.
Overview of Headache Types Based on Location
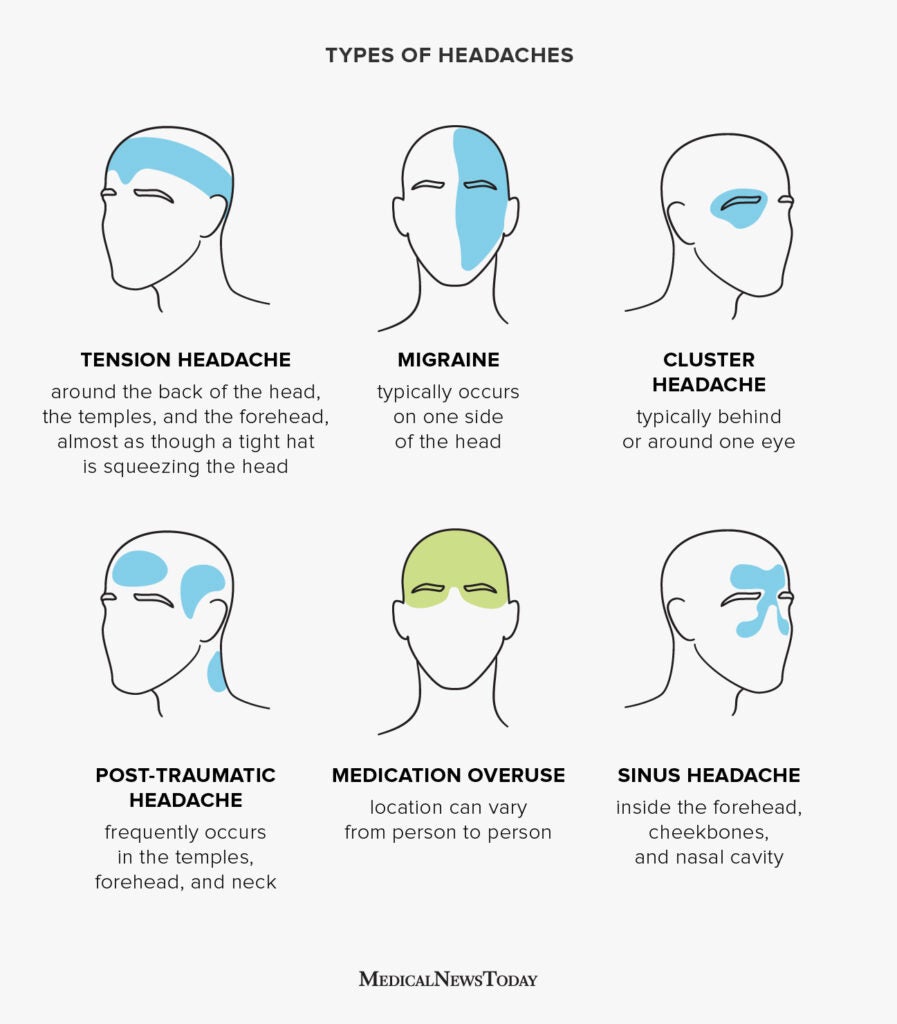
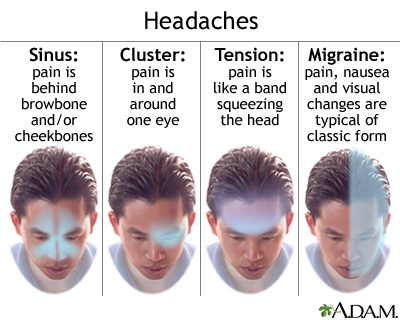
Understanding headache types based on their location can provide valuable insights into their potential causes and inform more effective treatment strategies. Here"s an overview of common headache types categorized by their primary locations:
- Frontal Headaches: Often associated with tension headaches, these can be caused by stress, poor posture, or eye strain.
- Temporal Headaches: Located on the sides of the head, these are typically seen in migraines and hormonal headaches, especially in women.
- Occipital Headaches: Found at the back of the head, indicating issues like cervicogenic headaches, which stem from neck problems, or tension from poor sleep positions.
- Headaches Behind the Eyes: Usually linked to sinus issues or cluster headaches, which can cause intense pain around or behind the eye.
- Dehydration Headaches: Can occur throughout the head and are easily remedied by increasing fluid intake.
- Cluster Headaches: Characterized by severe pain on one side of the head, often around the eye, with episodes occurring in clusters over weeks or months.
Each headache type may have distinct triggers and require specific approaches for management and relief. Recognizing the location and characteristics of your headache is the first step towards finding the most effective treatment.
Frontal Headaches: Tension and Sinus Related Causes
Frontal headaches, commonly experienced across the forehead, can be attributed to a variety of causes, with tension and sinus issues being among the most prevalent. Understanding these causes can aid in seeking appropriate treatment and relief.
- Tension Headaches: Often described as a tight band around the forehead, tension headaches are typically caused by stress, anxiety, or muscle strain. Factors such as poor posture, eye strain, or lack of sleep can also contribute.
- Sinus Headaches: Inflammation or infection of the sinuses can lead to pressure and pain in the frontal area. Symptoms may include a feeling of pressure across the forehead, cheekbones, and bridge of the nose, often accompanied by nasal congestion, facial swelling, and fever.
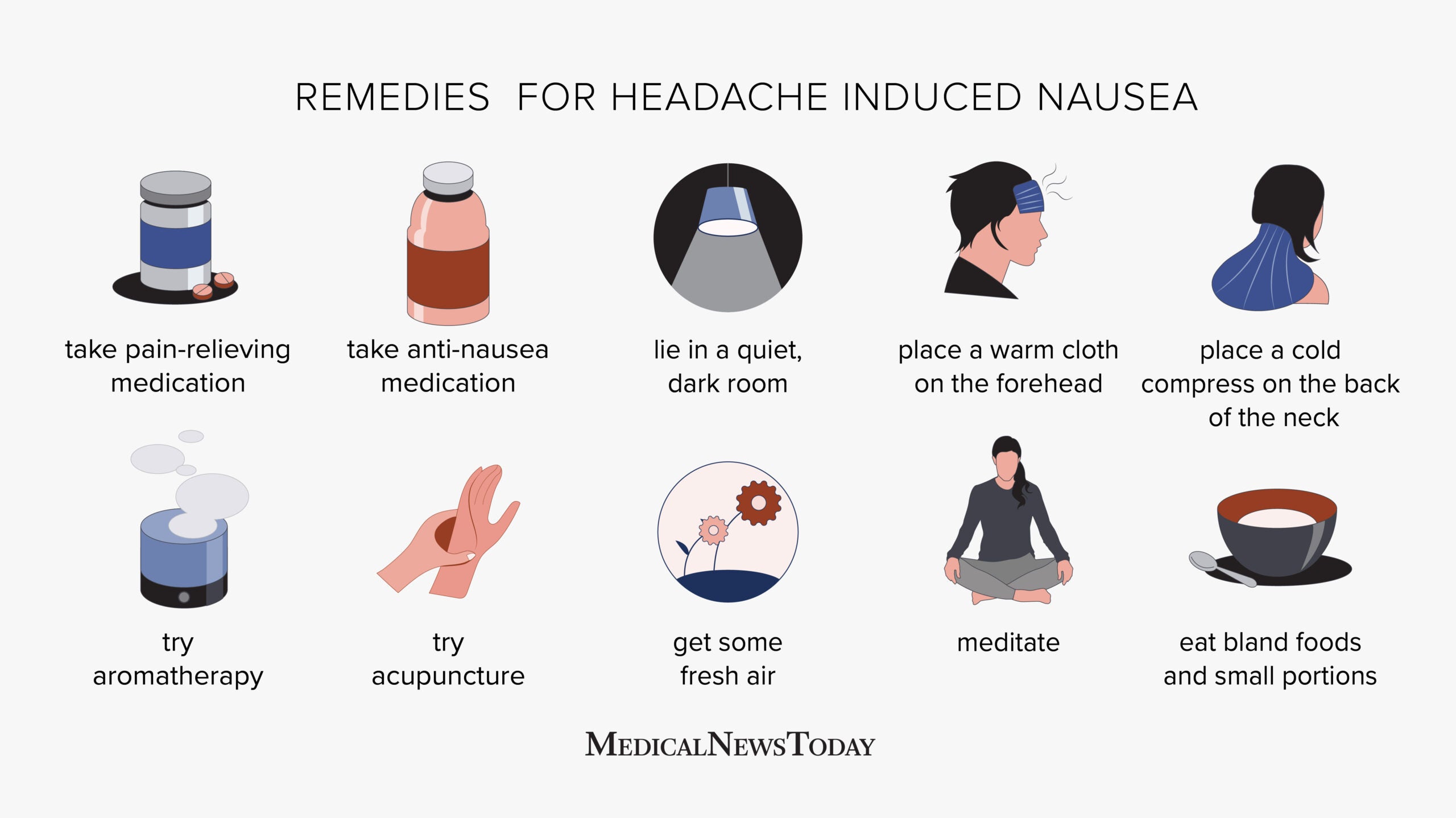
Both tension and sinus headaches can impact daily activities, but they can often be effectively managed with over-the-counter medications, proper rest, hydration, stress management techniques, and, in the case of sinus headaches, treating the underlying sinus conditions.
Headaches in the Temporal Area: Migraine and Hormonal Influences
Headaches in the temporal area are often linked to migraines and hormonal changes, providing distinct patterns that can help in diagnosis and treatment. Understanding these influences is key to managing and potentially reducing the frequency of these headaches.
- Migraines: Characterized by throbbing pain on one or both sides of the head, migraines in the temporal area can also include symptoms like nausea, light sensitivity, and visual disturbances. Triggers vary widely, including stress, certain foods, and environmental factors.
- Hormonal Influences: Fluctuations in hormones, particularly estrogen, can trigger headaches in the temporal area. This is especially common among women, who may experience increased headache activity during menstruation, pregnancy, or menopause due to changing hormone levels.
Identifying and avoiding triggers, along with medical or alternative treatments, can help manage the impact of temporal headaches. In some cases, preventive medications or lifestyle adjustments may also be recommended to reduce the occurrence of these headaches.

Occipital Headaches: Cervicogenic and Occipital Neuralgia
Occipital headaches arise from the back of the head, often signaling specific conditions such as cervicogenic headaches or occipital neuralgia. Understanding these conditions can guide effective management and relief strategies.
- Cervicogenic Headaches: Originating from the cervical spine or the base of the skull, these headaches are often the result of structural issues in the neck. Symptoms can include pain that radiates from the neck to the back of the head and sometimes to the eyes or behind the ears. Physical therapy, posture correction, and sometimes injections are part of the treatment regimen.
- Occipital Neuralgia: This condition involves inflammation or irritation of the occipital nerves, leading to sharp, shooting pains in the back of the head and neck. The pain can mimic other types of headaches, making accurate diagnosis crucial. Treatment may include nerve blocks, medication, and physical therapy.
Both conditions highlight the importance of accurately identifying the headache"s source for targeted treatment. Consulting with a healthcare professional skilled in diagnosing and managing head and neck pain is crucial for those suffering from these types of headaches.
Headaches Behind the Eyes: Cluster Headaches and Sinus Issues
Headaches located behind the eyes can be particularly distressing, often signaling either cluster headaches or sinus-related issues. Both conditions have unique characteristics and treatment approaches.
- Cluster Headaches: Known for their severe, piercing pain behind one eye, cluster headaches are rare but intensely painful. They occur in cyclical patterns or clusters, hence the name. These headaches may be accompanied by eye watering, nasal congestion, or eyelid drooping on the affected side.
- Sinus Issues: Sinus headaches, caused by sinusitis, lead to pressure and pain behind the eyes, cheeks, and forehead. These headaches often come with symptoms like nasal congestion, facial pressure, and a reduced sense of smell, and are typically triggered by infections or allergies.
While cluster headaches may require treatments like oxygen therapy, triptans, or preventatives, sinus headaches are often relieved by addressing the underlying sinus condition, possibly with decongestants, antibiotics, or nasal corticosteroids. Identifying the type of headache is crucial for effective treatment and relief.

Headaches Affecting the Entire Head: Dehydration and High Blood Pressure
Headaches that encompass the entire head can often be attributed to dehydration and high blood pressure, two conditions with widespread impacts on overall health.
- Dehydration Headaches: When the body loses more fluids than it takes in, dehydration headaches can occur. These headaches can feel like a dull, all-over pain or pressure. Increasing water intake and staying hydrated can help prevent and alleviate these headaches.
- High Blood Pressure Headaches: Although high blood pressure often presents no symptoms, severe cases can lead to headaches. The pain is typically felt on both sides of the head and can be accompanied by other symptoms like dizziness and nosebleeds. Managing blood pressure through lifestyle changes and medication is key to reducing these headaches.
Both conditions highlight the importance of maintaining overall health and well-being to prevent headaches. Regular check-ups, a balanced diet, and adequate hydration are essential preventative measures.
Understanding the Meaning of Headache Location
Headache: Are you tired of dealing with pesky headaches that just won\'t go away? Discover the ultimate solution to conquering your headaches with this informative video that\'s packed with effective tips and remedies. Say goodbye to headaches for good!
Decoding the Significance of Headache Locations
Locations: Have you ever wondered about the most breathtaking and unique locations around the world? Get ready for an awe-inspiring journey as you explore some of the lesser-known yet absolutely stunning locations in this captivating video. Get your wanderlust ready!
Understanding Cluster Headaches: Symptoms and Treatments
Cluster headaches are a type of headache that is marked by severe pain on one side of the head, often around the eye. They are called "cluster headaches" because they tend to occur in groups or clusters over a period of weeks or months, followed by periods of remission when the headaches stop. Understanding the symptoms and available treatments is crucial for those affected by this condition.
Symptoms of Cluster Headaches
- Intense pain on one side of the head: Typically, the pain is located around the eye, temple, or forehead. It is often described as sharp, burning, or piercing.
- Restlessness: Unlike migraine sufferers who prefer to lie down, those experiencing a cluster headache may feel restless and unable to stay still.
- Other symptoms: These can include a watery eye, nasal congestion, or a runny nose on the same side as the pain, eyelid drooping, and facial sweating.
- Short duration: Attacks can last from 15 minutes to 3 hours but occur one to three times a day during a cluster period.
Treatments for Cluster Headaches
Treatment for cluster headaches focuses on reducing the severity of pain during attacks and decreasing the frequency of the headache clusters.
- Oxygen therapy: Breathing pure oxygen through a mask can provide significant relief for most people during an attack.
- Medications: The use of certain medications, such as triptans (usually in injectable form) and corticosteroids, can help to alleviate symptoms or shorten the length of a cluster period.
- Preventive treatments: These may include the prescription of medications such as verapamil, a calcium channel blocker, which has been shown to reduce the frequency and intensity of cluster headaches for some patients.
- Lifestyle adjustments: Avoiding alcohol and smoking, maintaining a regular sleep schedule, and managing stress can help reduce the frequency of cluster headache periods.
- Surgical options: In rare cases where conventional treatments are not effective, surgical interventions that target specific nerves or brain areas involved in cluster headaches may be considered.
It"s important for individuals experiencing symptoms of cluster headaches to consult with a healthcare professional for a proper diagnosis and treatment plan. With the right approach, many people find relief from the pain and disruption caused by cluster headaches.
:max_bytes(150000):strip_icc()/headache-location-5215444_FINAL-3e29bd447744473dad2defe2db3ef14c.jpg)
Neck-Originated Headaches: Cervicogenic Headaches and Treatment Options
Cervicogenic headaches are a type of headache that originates from the cervical spine or the base of the skull. They are often caused by disorders of the neck, including misalignments, muscle tightness, and nerve compression. Recognizing the symptoms and understanding the treatment options can significantly improve the quality of life for those affected.
Symptoms of Cervicogenic Headaches
- Pain on one side of the head or face: The pain starts in the neck and then spreads to the head or face, usually on the same side.
- Neck movement triggers pain: The pain may worsen with certain neck movements or positions.
- Stiff neck: Reduced range of motion in the neck, along with muscle tightness.
- Other symptoms: May include sensitivity to light and noise, blurry vision, and nausea.
Treatment Options for Cervicogenic Headaches
Treating cervicogenic headaches often involves a combination of therapies aimed at alleviating pain and addressing the underlying causes.
- Physical therapy: Exercises and manipulations to improve neck posture, strength, and flexibility can reduce the frequency and intensity of headaches.
- Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may help relieve pain and inflammation.
- Injections: Nerve blocks or steroid injections can provide relief for those with severe pain.
- Manual therapies: Techniques such as massage, chiropractic adjustments, and osteopathy can help relieve symptoms.
- Heat therapy: Applying heat to the neck area can help loosen tight muscles and relieve pain.
- Lifestyle adjustments: Ergonomic modifications at work, proper posture, and stress management techniques can reduce the likelihood of headache triggers.
- Surgical intervention: In rare cases, surgery may be necessary to correct structural problems in the neck that cause headaches.
Collaborating with healthcare providers to develop a comprehensive treatment plan is essential. With appropriate management, individuals suffering from cervicogenic headaches can experience significant relief and improvement in their daily lives.
READ MORE:
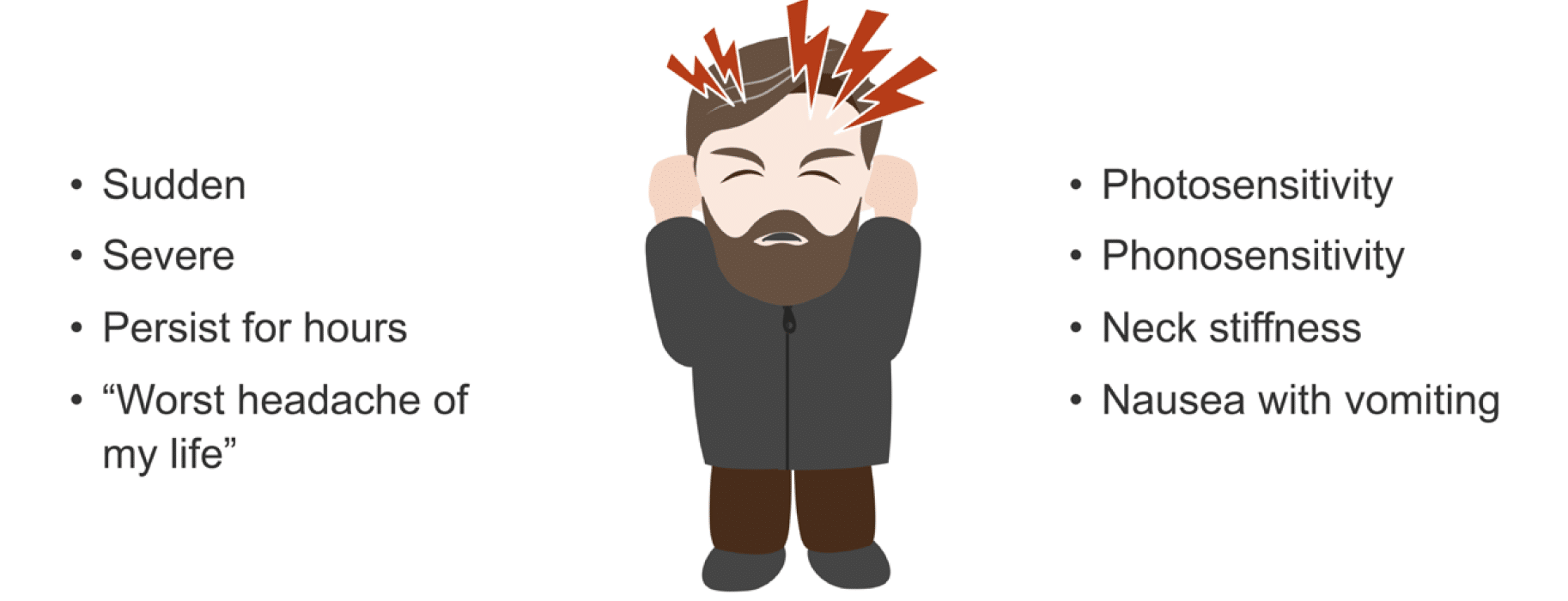
When to Seek Medical Attention for Your Headache
While headaches are common and often not a cause for alarm, there are situations where they can be a sign of a more serious condition. Knowing when to seek medical attention is crucial for your health and well-being. This guide will help you understand the warning signs that indicate a headache might require more than just over-the-counter medication.
Warning Signs That Require Immediate Medical Attention
- Sudden, severe headache: A headache that comes on suddenly and is more severe than any you"ve experienced before.
- Headache after a head injury: Especially if the headache gets worse, which could indicate a concussion or more serious brain injury.
- Changes in vision or speech: Difficulty speaking, or changes in vision, such as blurriness or double vision, accompanying a headache.
- Weakness or numbness: On one side of the body, which could be a sign of a stroke.
- Fever and stiff neck: Along with a headache, these symptoms can indicate meningitis, a serious infection that requires immediate treatment.
Other Reasons to Consult a Healthcare Professional
- Chronic headaches: If you experience headaches more than 15 days a month.
- Changes in headache pattern: Any significant change in the frequency, severity, or characteristics of your headaches.
- No relief from over-the-counter medications: Or if you find yourself relying on them more than twice a week.
- Interference with daily life: If headaches are disrupting your ability to work, sleep, or enjoy life.
Consulting with a healthcare professional can help you get a proper diagnosis and treatment plan. Whether your headaches are a symptom of a more serious condition or a manageable health issue, getting the right care is essential. Remember, you know your body best. If something feels wrong, it"s better to be safe and seek medical advice.
Understanding the meaning behind headache locations can empower you to identify potential causes and seek appropriate treatment. Let this guide be your first step towards managing your headaches effectively and improving your quality of life.


:max_bytes(150000):strip_icc()/Health-dehydration-symptoms-7480908-Horiz-e2500f0828b746ee9d2e2b5257af60cb.jpg)


:max_bytes(150000):strip_icc()/headache-on-the-right-side-5216756_final-b9d0145864d74706b0316a2e9b62dd37.jpg)
:max_bytes(150000):strip_icc()/vision-and-headache-3422017_final-f90b31917b244236a7424b143a537fd3.jpg)
:max_bytes(150000):strip_icc()/migraine-relief-pressure-points-5205811-FINAL-cdc9e0d051cb460bac8baa98bc01954f.jpg)